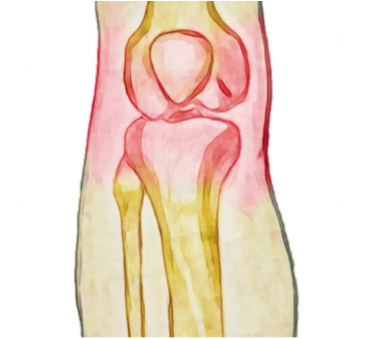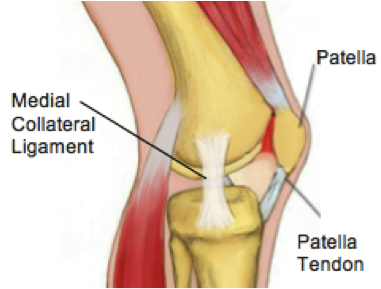
Knee pain comes in many forms with many different causes. While treatment for every person and condition will be different in each case, here are a few tips that may help to reduce knee pain throughout the day.
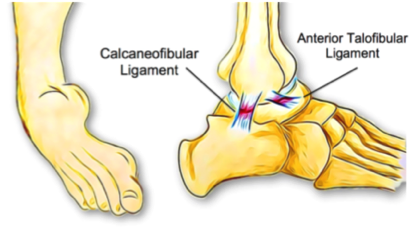
1. Choose supportive footwear
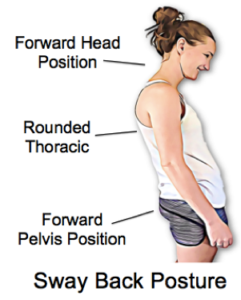
One of the biggest culprits for ongoing knee pain is wearing unsupportive or high-heeled shoes to work. High heels often lead to tight calves and altered gait patterns, while unsupportive shoes can allow rolling in of the ankles, which can, in turn, place extra stress on the knee joints. Having an assessment with your physiotherapist to see how your shoes might be affecting your knee pain is a worthwhile investment.
2. Adjust your sleeping position
While most of the time, our knees get a well-deserved rest during the nighttime hours, there are a few sleeping positions that can place additional stress on the knees. Lying on your side with bent knees can place tension on the outer thigh muscles and also the knee joint itself. Try to keep your knees straightened to at least 30 degrees and if you sleep on your side, place a pillow underneath the top knee to reduce stress on the joint.
Alternatively, if you sleep on your back it may be helpful to place a pillow under your knees so that they rest in a slightly bent position, to unload the joint. Try experimenting with different pillow arrangements to see which combination works best for you.
3. Avoid sitting or resting too much
When knee pain strikes, your first instinct is probably to get off your feet and stop exercising. The truth is that our knees, like all our joints, are designed for movement and regular exercise helps to keep them healthy. If you are having pain with high impact activities such as running, try switching to swimming and cycling before stopping exercise altogether. Resting in a sitting position for prolonged periods can also place excess stress over the knee cap and knee joint. When sitting for long periods, try to stretch your legs out ahead of you and avoid crossing your legs.
4. Seek physiotherapy treatment
Many of us see putting up with pain as a sign of strength however, a small niggle that is easily treatable can turn into a larger problem if left over time. This may seem like an obvious point, yet the first step to recovery is often just seeking treatment.
Our physiotherapist is happy to discuss your condition with you and share his tips to help you stay pain-free.