What is it?
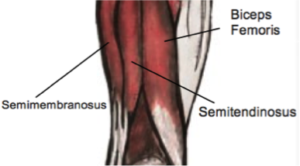
The hamstrings are a large group of muscles found at the back of the thigh. The primary role of these muscles is to bend the knee and collectively, these muscles are some of the strongest in the body. Despite their strength, the hamstrings are very prone to injury especially when overworked or undertrained. Hamstring strains and tears are quite common in sports that involving sprinting, jumping and sudden changes in speed. Football and soccer players are some of the athletes most commonly affected by hamstring tears.
Hamstring Muscles
Hamstring strains are categorized into three grades, these are:
Grade 1 (mild) – A few muscle fibers are either damaged or ruptured; there may be pain a day after the injury but no loss of movement.
Grade 2 (moderate) – Roughly half of the muscle fibers are torn; there may be acute pain and mild loss of function; walking may be affected. Grade 3 (severe) – More than half of the muscle fibers are ruptured and there is immense pain and swelling; definite muscle weakness and loss of function.
Grade 3 (severe) – More than half of the muscle fibers are ruptured and there is immense pain and swelling; definite muscle weakness and loss of function.
What are the symptoms?
The symptoms of a hamstring tear depend on the severity of the injury. Common symptoms include pain at the back of the thigh – which could range from mild to severe, swelling, bruising, loss of knee motion, tenderness at the back of the thigh, reduced length and muscle weakness of the hamstring. In some cases, tingling, numbness and weakness of the structures below the knee are seen. However, these are rare.
What are the causes?
A single cause of hamstring tears can be difficult to determine however, it is thought that a lack of coordination between the hamstrings and quadriceps muscles during sudden changes of speed or when kicking can cause the hamstrings to contract excessively or become overstretched, causing a tear.
There are also recognised risk factors, that increase the possibility of hamstring tears including increased age, fatigue, strength imbalance, previous injury of the hamstrings, poor core stability, poor hamstrings flexibility and tight hip flexors.
How can they be prevented?
Understandably, trying to prevent hamstring tears is important business. Research has consistently shown that the most important factor in preventing hamstring tears is having high eccentric strength in the hamstrings. Eccentric muscle contractions occur when a muscle is contracting while also lengthening. For example, when you lower your straightened leg slowly to the ground, your quadriceps muscle will be working eccentrically.
Your physiotherapists is able to show you some exercises that can target eccentric muscle strength specifically as well as identifying any risk factors that may be contributing to you individual risk. None of the information in this blog is a replacement for proper medical advice. Always see a medical professional for advice on your individual condition.