If you happen to have an office job, it can’t have escaped your notice that sitting has been shown to be associated with a variety of chronic health conditions. Office jobs are one the most common forms of employment in the developed world, so here are some tips to help you stay healthy when sitting all day.
Move more often:
Sitting itself and the posture you find yourself in isn’t as bad as simply being still for hours on end. An expression in physiotherapy is ‘the best posture is your next posture’. This means that, above all, movement is the best thing for your body and those in office jobs can find themselves becoming very still while focused on the next deadline.
Set a quiet alarm to remind you to move or change positions every 20 minutes. Getting up for phone calls and walking over to see colleagues when you have a question is a great way to break up your sitting time.
Reverse your posture:
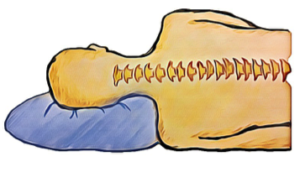
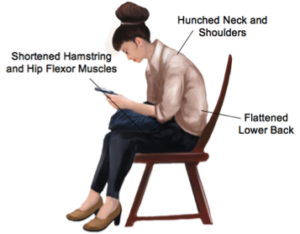
While not moving is definitely the worst aspect to prolonged sitting, the postures we often adopt while sitting can also be problematic. Sitting with a flattened lower back, hunched neck and slouched shoulders is the posture that requires the least energy to maintain and is often the one we sink into in a long day. A slouched posture can lead to shortened hamstring, hip flexor and pectoral muscles.
If you are spending large amounts of time sitting, it’s important to take time every day to adopt the opposite postures and keep your body flexible.
This means moving into thoracic and lumbar extension, stretching your shoulders and extending your hips.
Here are a few stretches you can do every day while seated that will help to reverse your posture. Try to do these stretches every few hours during a working day.
1.Chest stretch
Sit forward, clasp your hands behind your back and lift your arms towards the ceiling. You should feel a stretch at the front of your chest. Look up slightly to increase the stretch. You should not feel any pain or tingling in your arms. Hold for 30 seconds and repeat.
- Seated hamstring stretch
Perch on the edge of your seat and straighten one leg out in front of you. Lean forwards at your hips, keeping your back straight. You should feel a gentle stretch at the back of your thigh. If you feel the stretch behind your knee or into your calf, let your ankle relax, and let your foot drop towards the floor. Hold the stretch for 20 second then swap legs, repeat this stretch with each leg twice.
- Chin Tuck
Sit up in your chair so your bottom is at the back of your seat and your lower back is supported. Relax your shoulders and gently tuck your chin in, imagine you are holding a soft ball under your chin and are slowly squashing it. You should feel a gentle stretch at the top of your neck. Hold for 20 seconds, release and repeat.
You should not feel any pain with these stretches. Speak to your physiotherapist for a customised stretching routine that you can implement into your day at the office or for more tips on how to perform these stretches to maximum effect. None of the information in this article is a replacement for proper medical advice. Always see a medical professional for advice on your individual condition.