What is it?
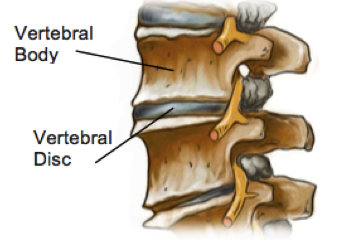
The discs of the spine sit between the vertebral bodies and act as shock absorbers for the spine. In the lumbar spine the outer part of the disc is made up of thick fibrous rings called the annulus fibrosus and the inner part is a soft jelly like substance called the nucleus pulposus. The discs in the spine also move to allow flexibility and movement of the spine, particularly in the lumbar spine where they are the largest.
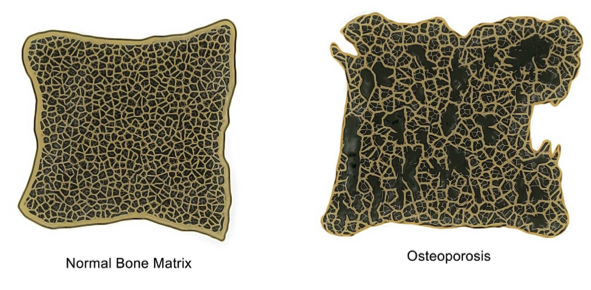
As we age, our discs begin to dehydrate, losing height, elasticity, and flexibility. The result is a spine that can feel stiffer, less flexible and a bit sore with certain movements. While almost everyone will have some degree of degeneration into their later years, not everyone will experience symptoms.
What are the Symptoms?
The most commonly felt symptoms of disc degeneration are stiffness and pain in the lower back. The pain is usually felt over the spine where the disc degeneration has occurred, but also often radiates into the buttock region. In severe cases of disc degeneration, increased wear and tear can cause bony spurs to develop on the vertebral body. These spurs can cause muscle weakness, numbness and tingling sensations in the leg and foot if they place pressure on the nerves around the spine.
How does this happen?
Disc degeneration usually affects people over the age of 50, however symptoms can begin in your 30s. As we age, all of our tissues gradually lose collagen and elastin, in the spinal discs this process results in smaller, less flexible discs. Repetitive activities like bending on the waist to lift heavy objects and prolonged sitting also cause additional wear and tear of the discs and amplify the degenerative process.
How Can Physiotherapy Help?
Imaging such as MRI and XRAY can help determine the level of degeneration that has occurred with increasing accuracy, however in recent years research has shown that the level of degeneration that can be seen In imaging cannot reliably predict the amount of pain a person will experience. This can be confusing for patients and having scans that show large amounts of degeneration can be a distressing experience, regardless of symptoms, making patients feel helpless.
Physiotherapy can help patients return to their normal activities as soon as possible and regain optimal function for their individual presentation. In addition, physiotherapy helps patients to manage their pain by helping them understand their pathology and, strengthen trunk stabilizers to prevent recurrence of any injury.
None of the information in this article is a replacement for proper medical advice. Always see a medical professional for advice on your individual injury.