Strains and sprains are words that are used almost interchangeably when describing injuries, however they each actually have quite distinct meanings. The most straightforward explanation is that a “strain” refers to a tear in a muscle or tendon, while a “sprain” refers to a tear in ligament fibers. Below we briefly describe what that means and how we treat sprains and strains differently.
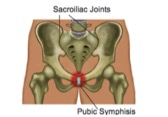
Ligaments are fibrous tissues that connect and hold bones to other bones. These are very strong parts of your anatomy and, depending on the joint, provide large amounts of support and stability to the body.
Some ligaments are so strong, for example in the shoulder, that sometimes a bone will break before the ligament will tear. When ligament fibers do tear, the nearby joint can actually feel unstable.
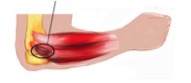
Ligament tears will usually swell up and have a normal inflammatory reaction. Pain will be worse with movement or if the ligament is placed under more stress. Occasionally, if a ligament has torn all the way through, there is much less pain than with a less severe injury.
Your physiotherapist is able to grade the severity of a ligament sprain, which will help guide treatment and expected recovery times. Muscle strains are easy to confuse with ligament sprains, however there are a few telltale differences. Following a muscle tear, it is more likely that you’ll feel weakness rather than instability. The pain will also be isolated over the muscle or tendon body. An injury to a ligament will be tender over the site of the ligament and special tests can be done to show a laxity due to the injury.
Treatment is also slightly different as sprains will need more support and will sometimes even need to be braced, whereas muscle strains will benefit from gentle movements earlier. In both cases, following the basic principles of rest, ice, compression and elevation is great advice in the early stages of any injury. Heat is not recommended until at least two days after the injury.
It is important to seek professional opinion when recovering from both a strain and a sprain. It is very easy to re-injure an area while it is healing if undertaking strenuous activity too early and without correct rehabilitation. Speak to your Matthew for more information.