If you are experiencing regular neck pain that just won’t go away, it’s possible that parts of your daily
routine are contributing without you realising. Here are a few common everyday activities that might be
making your neck pain worse.
Your sleeping position
It’s easy to underestimate the impact your sleeping position has however, spending hours in one
position will undoubtedly have an effect on your body. Pillows that are too high or too flat can mean
your cervical joints are sitting at the end of their range in too much flexion or extension. Similarly,
sleeping on your stomach often means your thoracic spine is locked into extension and your neck is fully rotated. In simpler terms, this means your joints are under more stress than necessary. Ideal sleeping posture allows your spine to maintain it’s natural curves.
Your daily commute
Many of us make sure our work stations are ergonomically set up to reduce stress and strain
throughout the day. Few of us take the same consideration when it comes to driving. In fact, the set up
of your car can be just as important as your work-desk, particularly if you are driving more than 30
minutes everyday. The correct setup in your car can mean you use less effort to drive and turn your
head less often to check traffic.
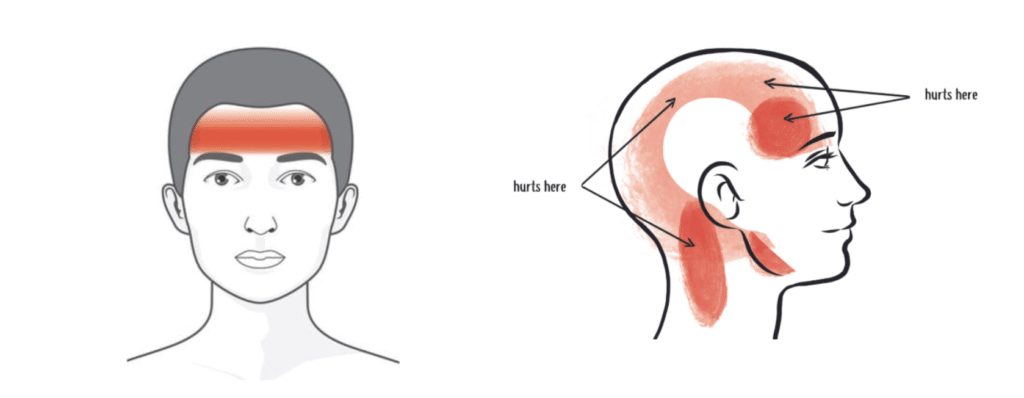
Ensuring that your steering wheel, seat and mirrors are set up correctly could make a difference to your
posture and even perhaps reduce neck pain and headaches. If you find that driving is still affecting your
pain after making these changes, try catching public transport or riding a bike on alternative days.
Your downtime
Many of us unwind by watching TV or our laptops at the end of the day. Your position during this time
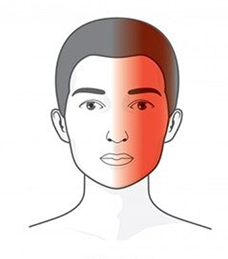
can be something you give little thought to however, looking up to view a screen mounted on a wall or
looking down at a small screen or laptop can put pressure on the upper structures of the neck. Take a
few minutes to consider what posture you’re sitting in before settling down to binge-watch a series and
see if you can either lower the height of your screen or raise it slightly so your neck can be in a more
neutral position.
Your exercise routine
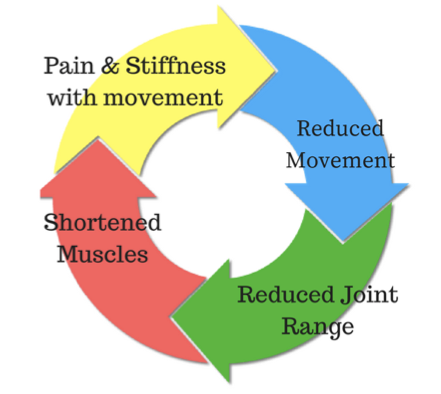
Any activity that requires sustained positions or repetitive neck movements can contribute to neck pain.
Cyclists can be stuck in neck extension while looking ahead and breast stroke swimmers can also have
excess neck extension. Freestyle swimmers with reduced thoracic or neck rotation can have difficulty
achieving rotation when breathing which can cause pain and discomfort over time.
Your physiotherapist Matthew West at Cumberland Physio Parramatta is able to identify any daily habits or activities that might be contributing to your neck pain.
Come and see us for an appointment to see how we can help.