Cumberland Physiotherapy Parramatta:
The start of the new year is an exciting time, where many of us feel inspired to set goals with the aim of improving our health, finances, and overall wellbeing. Many of us have tried to set goals before and found that, even with the best intentions, the newfound enthusiasm doesn’t last long and we end up back in old habits.
Here are a few tips to help you keep your New Year’s resolutions for longer and reach the goals you want to set for yourself.
Start before the new year
Many of us put off setting goals until New Years, especially with Christmas and New Years Parties making healthy living seem a little more out of reach. However, starting your resolutions earlier can actually be a great idea. This means you already have momentum once the new year arrives and are ready to continue on. Another benefit to starting your goals early that they will encourage you to go a little lighter throughout the holidays.
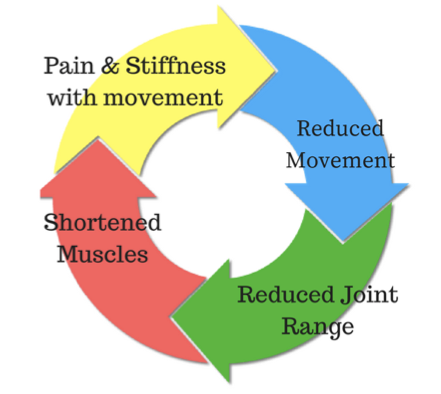
Let go of ‘all-or-nothing’ thinking
The problem with many diets and exercise programs is that once you miss a day at the gym or have a day of extra food or drinks, it is seen as failure. This can lead to feeling like giving up altogether. Strict regimes are both unrealistic and unhealthy, and don’t leave much room for fun or flexibility.
Track your progress
One of the best ways to stick to a new routine is to keep track of how often you show up. Start a checklist and tick off every day you stick to your new routine. It is often said that it takes 21 days for a new habit to form, which means that if you can keep it up for just 21 days, you’ve done most of the hard work.
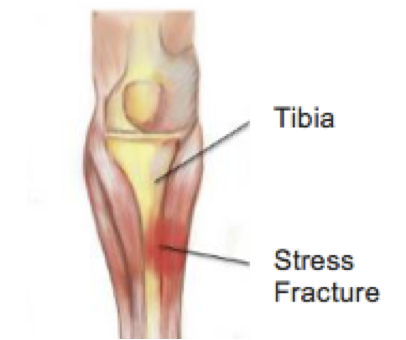
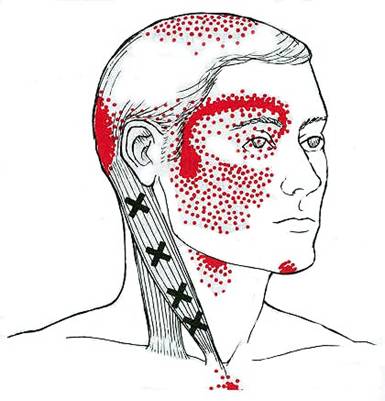
Get your niggles checked out
Nothing will stop a new exercise program faster than pain or injury. Unfortunately, small niggles often become more problematic when you start asking more from your body. Pop in to see your physio for advice on how to avoid injuries if you are taking up a new sport, and get those small aches and pains sorted early.
Ask our physio Matthew West at Parramatta for more tips on how to plan and stick to your New Years Goals. Happy New Year from our team!