From Cumberland Physiotherapy Parramatta:
What is Thoracic Outlet Syndrome?
The thoracic outlet is a small opening between the neck and shoulder that allows a variety of nerves and blood vessels to pass safely from the neck to supply the arm, chest, and shoulder blade. As this can be quite a small space, any narrowing can cause these structures to become compressed and irritated. This phenomenon is commonly referred to as thoracic outlet syndrome. This space can become compromised through trauma to the neck, overuse or repetitive stress to the arm, or the presence of an extra rib in the neck.
What are the signs and symptoms of Thoracic Outlet Syndrome?
Signs and symptoms of thoracic outlet syndrome may depend on whether nervous tissue or blood vessels are involved. In most cases, symptoms are caused by compression of nerve tissue rather than compression of veins or arteries.
When neural tissue compression is the cause of thoracic outlet syndrome, reported symptoms may include pins and needles, tingling, or numbness in the affected arm. Other symptoms include pain and weakness or tiredness in the arm that increases with overhead work. Some people may experience neck pain or headaches at the base of their head.
If a vein is affected, there may be swelling and discolouration of the affected arm, as well as pain.
When an artery is affected, cramping in the arm or hand during use may occur. Due to decreased blood flow, the arm or hand may feel cold and may even change colour.
Who is usually affected?
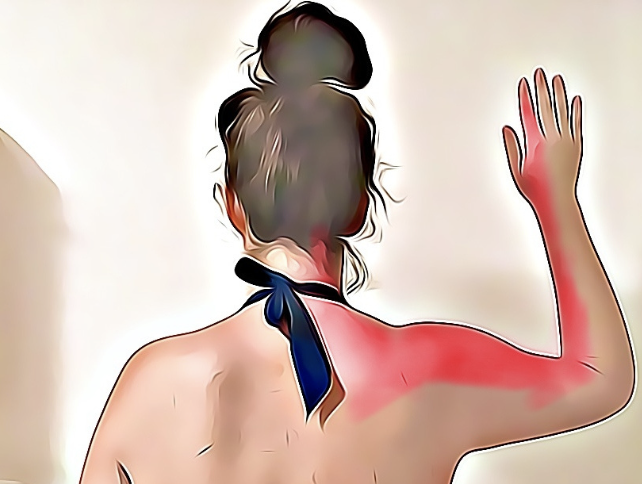
Thoracic outlet syndrome is more common in people who work with their arms in an above-shoulder position. For example, a teacher who writes frequently on a chalkboard, a construction worker hammering nails overhead, or a hairdresser.
How can physiotherapy help?
Our physiotherapist Matthew West at Cumberland Physio Parramatta will assess a range of factors, including your posture, the flexibility of your spine, and the length of your neck muscles. It is also important to assess how you move your neck, back, and arms.
Depending on the findings of the physical assessment, your physiotherapist may help you stretch appropriate muscles, modify movement patterns, and improve posture. This may involve manual therapy techniques such as joint mobilisations, strapping techniques, and soft tissue massage.
Treatment time may vary depending on symptom presentation and response. Thoracic outlet syndrome can take anywhere from a few treatments to several weeks to improve, along with continuation of a home exercise programme.
None of the information in this article replaces proper medical advice. Always consult a medical professional for advice about your individual condition.