CUMBERLAND PHYSIOTHERAPY PARRAMATTA:
What is it?
Vertigo, the feeling that you are moving even though you aren’t, is an unpleasant yet common experience caused by a variety of conditions. It may surprise you to learn that in some cases your physiotherapist is actually able to treat vertigo.
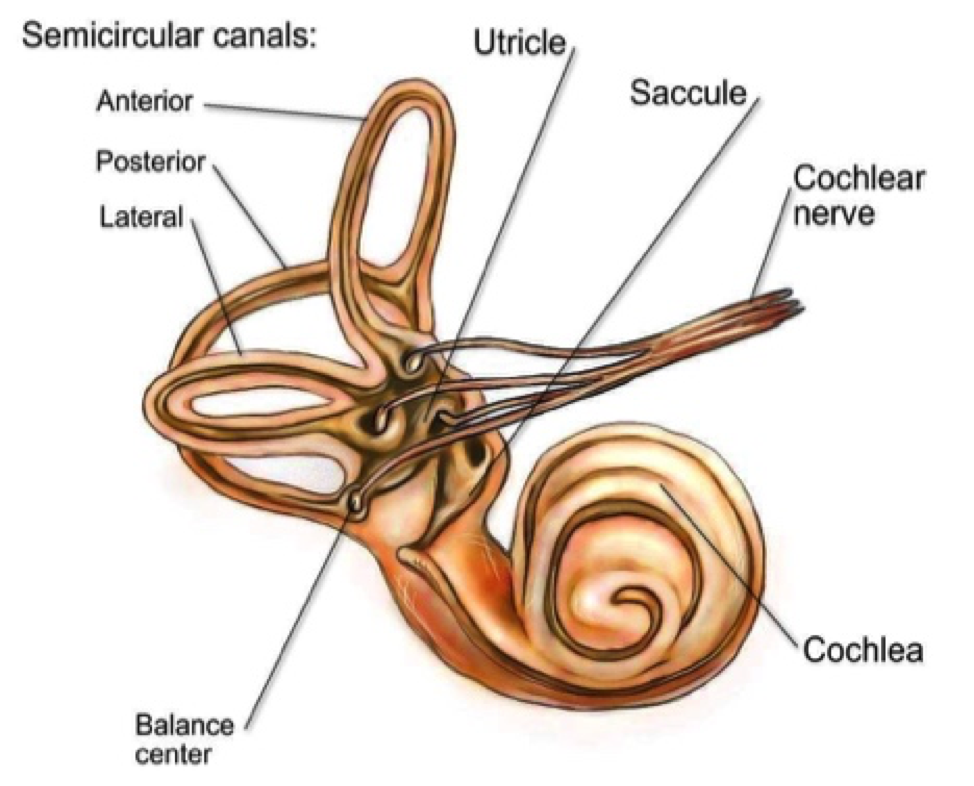
The process of telling whether we are moving or still involves many parts of the nervous system, including the inner ear. The vestibulocochlear nerve sends information about head movement to the brain, where it is processed. However, certain conditions can disrupt this process, causing the brain to perceive movement when there is none. Physiotherapists may be able to help with a specific type of vertigo called Benign Paroxysmal Positional Vertigo (BPPV).
What are the symptoms?
BPPV, also known as positional vertigo, causes dizziness only when the head moves in certain positions or directions. People with BPPV often experience dizziness and nausea when rolling over in bed or looking upwards, as well as lightheadedness and disturbance of balance. While BPPV can occur for no reason, it is often seen after a recent head trauma, respiratory infection, or airplane travel, as these conditions can disrupt the inner ear’s normal function.
How does it happen?
The symptoms of BPPV can be explained by a disruption in the signal sent by the semi-circular canals of the inner ear to the brain. These canals are positioned in different directions and filled with fluid. As the head moves, the fluid in each canal moves differently, depending on the head’s orientation. Receptors pick up this movement direction and speed, sending the message to the brain. However, sometimes small calcium crystals in the utricle, where the three semi-circular canals meet, can become dislodged and move into the semi-circular canals, disrupting the fluid and obscuring the messages to the brain.
What is the treatment?
If your doctor has diagnosed you with BPPV, they or your physiotherapist can show you a series of movements to help dislodge the calcium crystals and move them away from the semi-circular canal. You may also be asked to perform exercises to prevent the crystals from returning. Usually, only one or two treatments are needed for symptom resolution, although some cases may require more.
If you think you have vertigo, it is important to be assessed by a medical professional, as there are many conditions that can cause these symptoms and correct diagnosis is necessary before treatment. None of the information in this article is a replacement for proper medical advice. Always see a medical professional for advice on your condition.