CUMBERLAND PHYSIOTHERAPY PARRAMATTA: Maintaining balance is a complex process that your body does automatically. The body uses various systems to maintain balance, and if one system fails, the others compensate to keep you stable. You may not notice a deterioration in your balance until you’re in a challenging situation
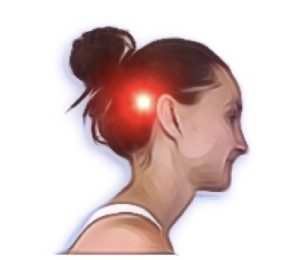
Our bodies have three systems that work together to keep us balanced: our vision, our inner ear, and our ability to sense the position and movement of our joints, muscles, and tendons, known as proprioception. Our eyes provide visual information about the world around us, while the inner ear helps us maintain our balance by detecting changes in our head’s position. Meanwhile, receptors in our joints, muscles, and tendons help us understand where our body is in space and how it is moving.
Poor balance can cause falls, broken bones, and serious injuries. The good news is that you can usually improve your balance with just a little practice. Here are a few quick tips you can try.
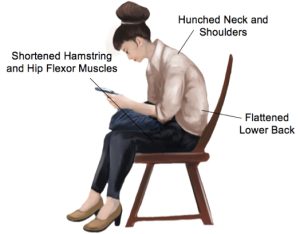
1. Maintain good posture: Good posture helps align your body, which is important for balance. Stand up straight with your shoulders back and head up. Avoid slouching or leaning to one side as it can throw off your balance.
2. Practice standing on one leg: Standing on one leg may seem easy, but it can be challenging if you’re not used to it. Start near a wall or hold onto a sturdy surface for balance. Gradually try standing on one leg without support. This exercise improves proprioception, which is your body’s ability to sense where it is in space.
3. Strengthen your core muscles: Core muscles located in your abdomen, back, and hips help stabilize your body and keep you upright. Strengthening them through exercises like planks, side planks, and bridges can improve your balance.
4. Regularly Challenge your balance: Notice what the limits of your balance are and see if you can improve on this gradually every day. Setting small goals for yourself can result in large improvements in your balance over time.
Talk to your physiotherapist about creating a personalised program to improve your balance. Your physiotherapist is an expert who can evaluate which aspects of your balance need improvement and how to do it. They can assess which exercises are most appropriate for you, regardless of your fitness level or age.