There is no doubt that the human body can be very resilient. Short of regenerating new limbs, our bodies are capable of recovering from large amounts of damage, including broken bones. With this in mind, many people are happy to let nature take it’s course following an injury, thinking that seeing a physiotherapist will only act to speed up already healing tissues.
The speed of recovery, however, is only one measure of healing and despite our bodies’ incredible capacity for repair; injury repair can be less than straightforward. Here are a few things about injury healing you may not have been aware of.
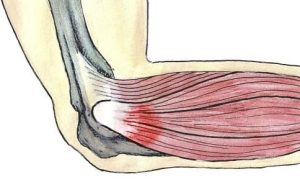
1. Scar Tissue is more likely to form without treatment.
Scar tissue can cause ongoing pain and stiffness in skin, muscles and ligaments. Physiotherapy can prevent excessive scarring from forming through advice regarding movement, massage and other hands-on treatment.
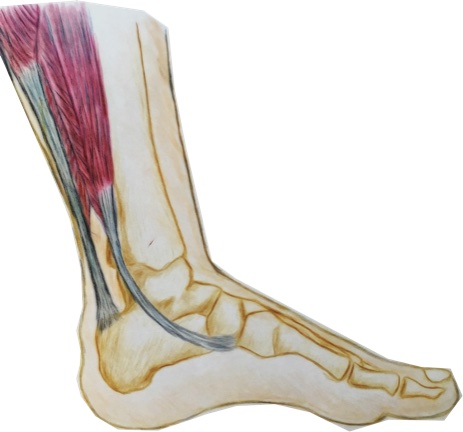
2. Your ability to sense the position of your body, known as proprioception, is often damaged after an injury and can be retrained.
Impaired proprioception is a major factor in re-injury. If you’ve ever heard someone say “my knee/ankle/shoulder still doesn’t feel 100%” then this could be why. The good news is that with a specific exercise program, proprioception can be improved and recovered.
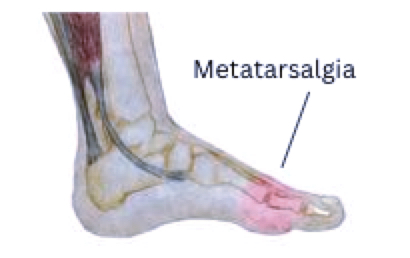
3. Once healing has finished, your body may not be exactly the same as before.
Following an injury, ligaments may be lax, joints may be stiffer and muscles are almost always weaker. While the pain may be gone, there might still be factors that need to be addressed to prevent more complicated issues in the future.
4. You may have picked up some bad habits while waiting for the injury to heal.
While in pain, we often change the way we do things, this can lead to the development of poor movement patterns and muscle imbalances. Even though the pain has gone, these new patterns can remain and create further problems down the road.
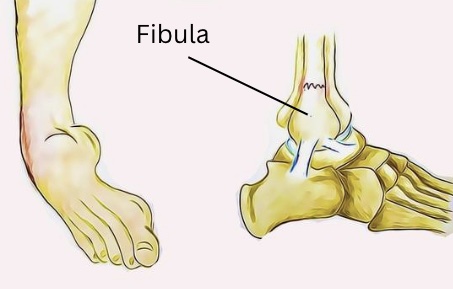
5. Injuries don’t always heal completely.
On rare occasions, injuries may not be able to heal completely on their own. The most serious example of this is a fracture that cannot heal if the bone is not kept still enough. Other factors that may prevent an injury from healing include poor circulation, diabetes, insufficient care of the injury and poor nutrition.
Your physiotherapist can assess your injury and develop a treatment plan that will both restore you to the best possible function and prevent further injuries. None of the information in this article is a replacement for proper medical advice. Always see a medical professional for advice on your individual injury.