What Is It?
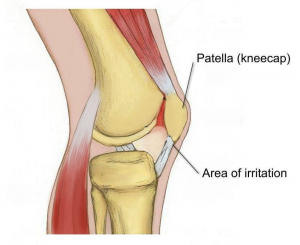
The knees function as hinges, allowing your legs to swing forwards and backwards smoothly as you walk, kick and run. The kneecap, also known as the patella, sits at the front of the knee and has a variety of functions, including guiding the muscles that straighten the knee, protecting the knee joint and absorbing forces when the knee is bent. When something goes wrong and the kneecap doesn’t move up and down smoothly, the soft tissue between the kneecap and the knee can become irritated, causing pain in a predictable fashion. This is called patellofemoral pain syndrome (PFPS), sometimes also referred to as PFJ syndrome or runner’s knee.
Pain is usually felt on the inside of the kneecap when you put pressure on your knees by running, squatting, bending, using stairs, or hopping. Sitting for long periods of time or keeping your knees bent could also result in pain.
What Causes It?
The kneecap sits in a shallow groove at the front of the knee and usually moves up and down as the knee bends and straightens without too much trouble. The quadriceps muscles, located at the front of the thigh, contract and pull on the kneecap, which then attaches to the lower leg and act to straighten the knee. If one side of the quadriceps is stronger or tighter than the other, it can cause the kneecap to pull to one side and over time become irritated.
The cause of muscle imbalance or weakness can be for many reasons. In general, the outer muscles of the thigh tend to be stronger and tighter than the inside muscles. If you have poor posture and hip position, this often causes the outer muscles to work harder and the inside muscles to become weaker. Lack of arch support in your feet or simply a physical abnormality of the knees can also cause this condition.
How Can Physiotherapy Help?
Diagnosing patella-femoral pain syndrome correctly is important because pain on the inside of the knee can also be caused by injury, dislocation, inflammation, arthritis and a variety of other less common diseases.
With that in mind, it is helpful to know that your physiotherapist can diagnosis PFPS and identify its likely causes.
Whether it is due to poor posture, a lack of arch support in your feet, or poor running technique, your physiotherapist will assess the problem and provide a specific treatment program to best approach your condition. PFP syndrome usually responds quite well to biomechanical analysis and correction of any muscular weakness and imbalance. Having the correct shoes and orthotics can also make a huge difference. There are some short-term treatments, such as patella taping, try needling, trigger point therapy and ultrasound, which may help alleviate symptoms quickly and keep you active while you address the other factors contributing to your pain.
In the rare case that your condition is not helped by physiotherapy, surgery is also considered as last resort. For more information, please feel free to ask your physiotherapist.
None of the information in this article is a replacement for proper medical advice. Always see a medical professional for advice on your individual injury.