What are they?
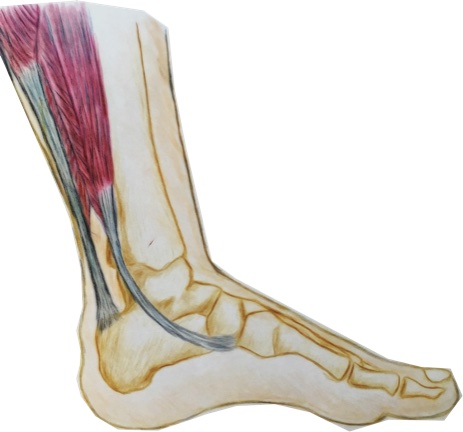
The calf muscles refer to a group of muscles at the back of the lower leg that act to point the foot away from the body and play an important role in walking and running. A tear or strain of these muscles occurs when some or all of the muscle fibres are torn or stretched. This is a common injury that can affect anyone from athletes to those with a more relaxed lifestyle.
How do they happen?
Calf tears are often caused by sudden, forceful movements or overuse of the calf muscles, leading to the rupture or strain of muscle fibres. Common mechanisms of injury are a quick take off during a sports match or simply going for a long walk when not accustomed. Factors that may increase the risk of a calf tear are previous calf tears that have not been fully rehabilitated, tight and weak calf muscles, poor balance and ill fitting footwear.
What are the symptoms?
Typical symptoms of a calf tear are sharp pain over the site of the tear, especially with movement, swelling, bruising, and difficulty walking or standing. The severity of the injury can range from mild muscle strain to a complete tear, which will determine the appropriate treatment approach.
How can physiotherapy help?
The first step in managing calf tears is accurate diagnosis by a medical professional, who is able to rule out other conditions that might mimic a calf tear. They can determine the extent of the damage and create personalised treatment plans based on the patient’s specific needs. This ensures that the rehabilitation process addresses the root cause of the injury, leading to better outcomes.
Reducing pain and inflammation is important in the first one to two days following the injury. The muscle may need support during this time, depending on the severity. Over time as the swelling and inflammation subsides, your physiotherapist will help to address any factors that contributed to the injury such as muscle weakness or imbalance. Calf tears often lead to stiffness and limited range of motion in the affected leg.
Physiotherapists implement targeted stretching and range of motion exercises to restore flexibility and prevent the formation of scar tissue that may impede recovery. Gradually, the patient can regain the ability to move the calf muscle without pain or discomfort.
Rehabilitation past this point will progressively challenge the calf muscles without causing further damage. Strengthening these muscles not only aids in the healing process but also reduces the risk of future calf tears.
Proprioception, the body’s ability to sense its position in space, is crucial for balance and coordination. Physiotherapy includes specialised exercises that enhance proprioception and balance, reducing the likelihood of re-injury. This aspect of rehabilitation is especially important for athletes and active individuals who need to return to high-intensity activities safely.
None of the information in this article is a replacement for proper medical advice. Always see a medical professional for advice on your individual condition.