One of the most challenging aspects of living with an injury or chronic pain is how it can quickly impact your exercise routine. If you have been working towards a fitness or weight goal, this can be extremely demoralising. Here are a few tips that can help to keep you on track while you recover. Staying as active as possible during this time can mean you’re in the best position to reach your goals again once your injury has healed.
1. Try a new activity.
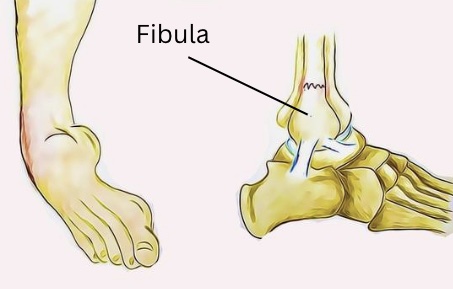
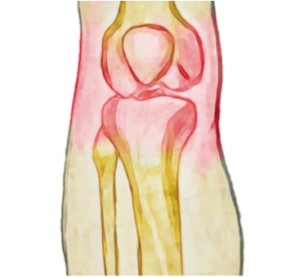
When injury strikes, it can be tempting to stop exercising altogether and rest while you recover. An injury can be frustrating, but it can also be an opportunity to try out a different sport. If you’re a runner with an ankle injury, you can keep up your fitness by swimming instead. Cycling can be an excellent option for people for dealing with knee pain, and if you’re a swimmer with shoulder pain, maybe switch to running for a while. Check with your physiotherapist for some ideas to keep you moving.
2. Exercise within your limits.
If you’re getting pain at 5km, this doesn’t always mean you should give up running altogether. Your physiotherapist can help you monitor your symptoms carefully and plan an exercise routine that keeps your fitness up while reducing symptom flare-ups. Staying as active as possible throughout your recovery can also mean that you a better placed to get back to your best performance once symptoms reside
3. Take the opportunity to improve your footwear and equipment.
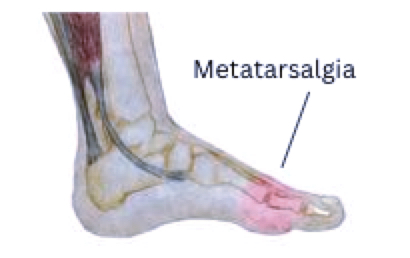
Injury and pain can be a great prompt to look at your equipment and technique . For example, with hip and knee pain, the type of shoes you wear can have a significant difference. Often pain has more than once cause, with technique and equipment more often than not having a substantial impact on the stress placed on your body. Your physiotherapist is an excellent source of advice in this area, don’t hesitate to ask for an assessment.
4. Take to the water
Hydrotherapy has long been used to help patients with joint pain or muscle weakness exercise. The water helps reduce joint stress and provide extra sensory input that can reduce pain. Exercising in water can be especially helpful for sufferers of chronic pain or those who have pain with weight-bearing. Speak to your physio for a hydrotherapy program if you’re not sure how to approach exercise in water.
Our physiotherapists are happy to discuss your condition with you and share their tips to help you stay pain-free. None of the information in this article is a replacement for proper medical advice. Always see a medical professional for advice on your condition.